Spirituality as a Facilitator for Recovery from Traumatic Brain Injury
Seibert Lab Seibert Lab
St. Alphonsus Medical Center & Physician Research
Boise, ID
Each year 1,500,000 individuals are diagnosed with a traumatic brain injury (TBI) and there are 3,170,000 individuals currently living with a traumatic brain injury in the United States.1 Globally, traumatic brain injury is the leading cause of death and disability worldwide.2 Traumatic brain injury critically impacts psychosocial neurological functioning as well as severe neurocognitive deficits. Patient recovery and outcomes vary dramatically even when injury type, location and severity are similar.3 Thus, it appears treatment modalities and injury severity are insufficient to explain the variance and divergence in patient outcomes and recovery. Spirituality has increasingly been reported as an important factor in successful recovery from various physical and psychological impairments, but its efficacy in aiding with patient recovery and improvement post-TBI has been largely understudied. Spiritual therapies have greatly improved psychosocial functioning and physical health and yet traditional medical institutions and therapeutic techniques often overlook and discount the important role spirituality plays in improving patient outcomes. The TBI subpopulation would especially benefit from the benefits and advantages spiritual therapy can offer, as the long term effects from a TBI can last the entirety of an individual’s life.
We assembled an interdisciplinary team and constructed a database comprised of 671 measures collected in 13 categories, including general demographics, injury event, brain injury type, medical treatment and care, social/family data, rehabilitation, cognitive research measures, post-injury follow-up data, outcome scores, and perspectives of spirituality effects and changes.
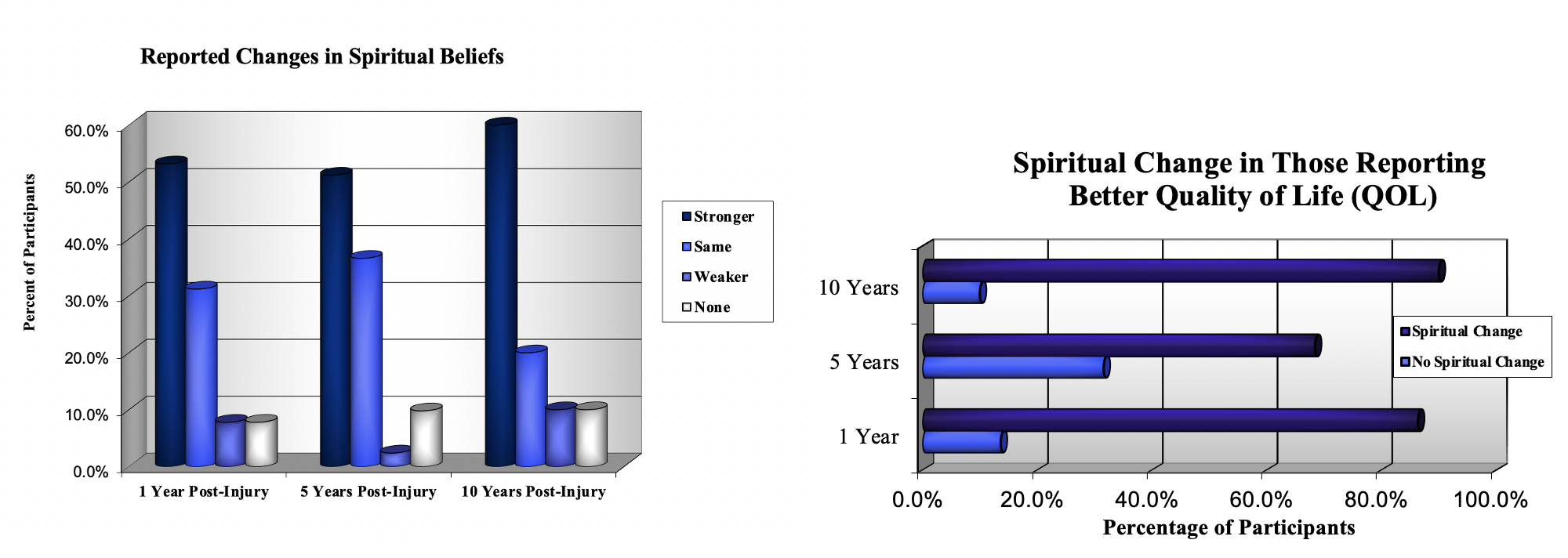
Data was analyzed to evaluate the role of spirituality in recovering from a TBI. Participants were asked two questions concerning spirituality. First, participants were asked to compare their spiritual life to before their injury and rate it on a scale of stronger, same, weaker, or none. Then they were asked if they experienced spiritual change. We also analyzed the participants’ perceived quality of life (QOL). At 1 year post-TBI, 30.1% reported a better QOL since the injury. At 5 years, 48.8% of the participants reported a better QOL. This increased yet again at the 10 year follow-up to 50% of the population. Furthermore, evidence supports the association between a better quality of life and spiritual change.
Acknowledging, assessing, and incorporating spirituality into the care plan is critical in helping to improve quality of life and quality of care. Our results demonstrate the influence that spirituality may have on recovery and improved quality of care post-TBI. Therefore, we intend to expand our study to further investigate the underlying facets of spirituality and its effects on TBI recovery and improved patient care. Clinicians and medical professionals should implement and assess spirituality as an important facet of the medical care plan and make resources available in order to encourage spiritual growth and development.
Dr. Seibert presented at American Association of Neurological Surgeons
Pennie S. Seibert, Ph.D., Colleen Poulton, Elora Williams, Christian Zimmerman, MD, MBA, FACS